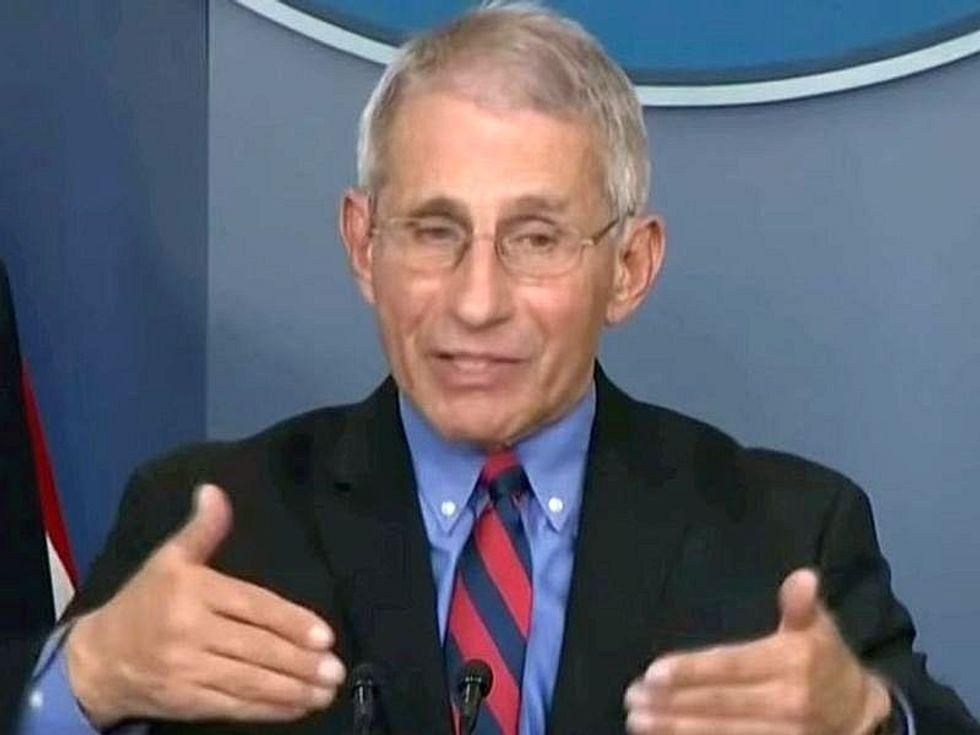
In an effort to avoid another pandemic in the coming years, Dr. Anthony Fauci wants to launch an ambitious plan to make prototype vaccines that could protect against pathogens from 20 families of viruses that threaten human lives.
It won’t come cheap, with the cost totaling “a few billion dollars” a year, Fauci said, and the first round of results wouldn’t emerge for at least five years. Also, a huge number of scientists would be needed to conduct the necessary studies.
“It would require pretty large sums of money,” Fauci told The New York Times. “But after what we’ve been through, it’s not out of the question.”
Using research tools that have worked with COVID-19, scientists would study the molecular structure of each virus, searching for the spots where antibodies must strike it, and figuring out how to prompt the body to make those antibodies.
“If we get the funding, which I believe we will, it likely will start in 2022,” Fauci said, adding that he has been pushing the idea “in discussions with the White House and others.”
Dr. Francis Collins, director of the U.S. National Institutes of Health, said he thought the necessary funds would be allocated and added that the project is “compelling.”
“As we begin to contemplate a successful end to the COVID-19 pandemic, we must not shift back into complacency,” Collins told the Times.
Much of the financial support would come from the agency that Fauci heads, the National Institute of Allergy and Infectious Diseases (NIAID), but additional funds that would have to be allocated by Congress, the Times reported. The institute’s budget is a little over $6 billion this year.
If a new virus was detected spilling over from animals into people, scientists could immunize people in the outbreak by quickly manufacturing the necessary prototype vaccine.
“The name of the game would be to try and restrict spillovers to outbreaks,” Dr. Dennis Burton, a vaccine researcher and chairman of the department of immunology and microbiology at Scripps Research Institute, told the Times.
The prototype vaccines project is the brainchild of Dr. Barney Graham, deputy director of the NIAID’s Vaccine Research Center. He presented the idea in February of 2017 at a private meeting of institute directors, the Times reported.
Year after year, viruses had threatened to turn into pandemics, Graham noted: the H1N1 swine flu in 2009, Chikungunya in 2012, MERS in 2013, Ebola in 2014, Zika in 2016. Each time, scientists scrambled to try to make a vaccine. Their only success was a partial one, with an Ebola vaccine that helped control the epidemic but would not work against other Ebola strains, he said. The other epidemics waned before vaccines could be made or tested.
But researchers now have new tools developed over the past decade that allowed scientists to view the molecular structures of viruses, isolate antibodies that block the viruses, and then find out where they bind. The result: An ability to target each emerging pathogen more precisely.
When he heard Graham’s pitch in 2017, Fauci was inspired. “It struck me and others in the executive committee as something that is really doable,” Fauci told the Times.
Now, the institute has created a spreadsheet for each of the 20 virus families showing what is known about each pathogen’s anatomy and vulnerabilities, Dr. John Mascola, director of the Vaccine Research Center at the institute, told the Times.
“For each virus family, we are in a different state of knowledge and vaccine development,” Mascola said. Vaccines for Lassa fever and Nipah virus, for example, are in early stages. Vaccines for Chikungunya and Zika are further along, the Times reported.
Vaccinations Start to Climb in States Hit Hard by Delta Variant
In a sign that vaccine-hesitant Americans are starting to worry about the rapid spread of the highly infectious Delta variant, vaccinations are beginning to rise in some states where COVID-19 cases are soaring, White House officials said last week.
Coronavirus coordinator Jeff Zients told reporters that several states with the highest proportions of new infections have seen residents get vaccinated at higher rates than the nation as a whole. Officials cited Arkansas, Florida, Louisiana, Missouri and Nevada as examples, the Associated Press reported.
“The fourth surge is real, and the numbers are quite frightening at the moment,” Louisiana Gov. John Bel Edwards said on a New Orleans radio show, the AP reported. “There’s no doubt that we are going in the wrong direction, and we’re going there in a hurry.”
On Thursday, Louisiana reported 2,843 new COVID-19 cases, one day after reporting 5,388 new infections — the third-highest level since the pandemic began. Hospitalizations are also up steeply in the last month, from 242 on June 19 to 913 in the latest report, the AP said. Just 36% of Louisiana’s population is fully vaccinated, state health department data shows.
Warner Thomas, president and CEO of the Ochsner Health system serving Louisiana and Mississippi, told the AP that the system had seen a 10% to 15% increase in people seeking vaccination over the past week or two. It has administered vaccines at churches, the New Orleans airport, basketball games and the mall.
“We see each person we get vaccinated now as a victory,” said Dr. Katherine Baumgarten, director of infection prevention and control for the 40-hospital system.
Missouri, which is second only to Arkansas and Louisiana in the number of new cases per capita over the past 14 days, lags about 10 percentage points behind the national average for people who have received at least one shot, the AP reported.
The case surge that began in the southwest part of that state has started to spread to the Kansas City area, including at Research Medical Center.
“I don’t want to keep putting my life on the line just because people don’t want to get vaccinated or listen to what health care professionals are recommending,” Pascaline Muhindura, a registered nurse who has worked on the hospital’s COVID-19 unit for more than a year, told the AP.
“A lot of them don’t even believe in COVID-19 to begin with. It is incredibly frustrating. You are helping someone that doesn’t even believe that the illness that they have is real,” Muhindura said.
Dr. Jason Wilson, an emergency physician with Tampa General Hospital in Florida, also has watched the rise in cases with frustration, the AP reported. Unlike earlier in the pandemic, when many patients were in their 70s, he has seen the median patient age drop to the mid-40s.
“This Delta [variant], at the moment, it is honing in on largely unvaccinated persons,” Dr. William Schaffner, a professor of infectious diseases at Vanderbilt University’s School of Medicine in Nashville, told the AP.
The variant, which first emerged in India, now accounts for an estimated 83% of coronavirus samples genetically identified in the United States. It is the predominant strain in every region of the country and continues “spreading with incredible efficiency,” Dr. Rochelle Walensky, head of the U.S. Centers for Disease Control and Prevention, told reporters at the White House on Thursday.
She called the Delta variant “one of the most infectious respiratory viruses we know of.”
More information
The U.S. Centers for Disease Control and Prevention has more on COVID-19.
SOURCES: Associated Press; The New York Times
Source: HealthDay

Leave a Reply