New research suggests that gender and money matter when it comes to getting a last-resort treatment after mechanical ventilation.
Funded by the U.S. National Institutes of Health, the study found that certain groups are more likely to receive advanced pulmonary support through ECMO (extracorporeal membrane oxygenation).
Who is more likely to get it? Men, those with higher incomes and those with health insurance, investigators discovered.
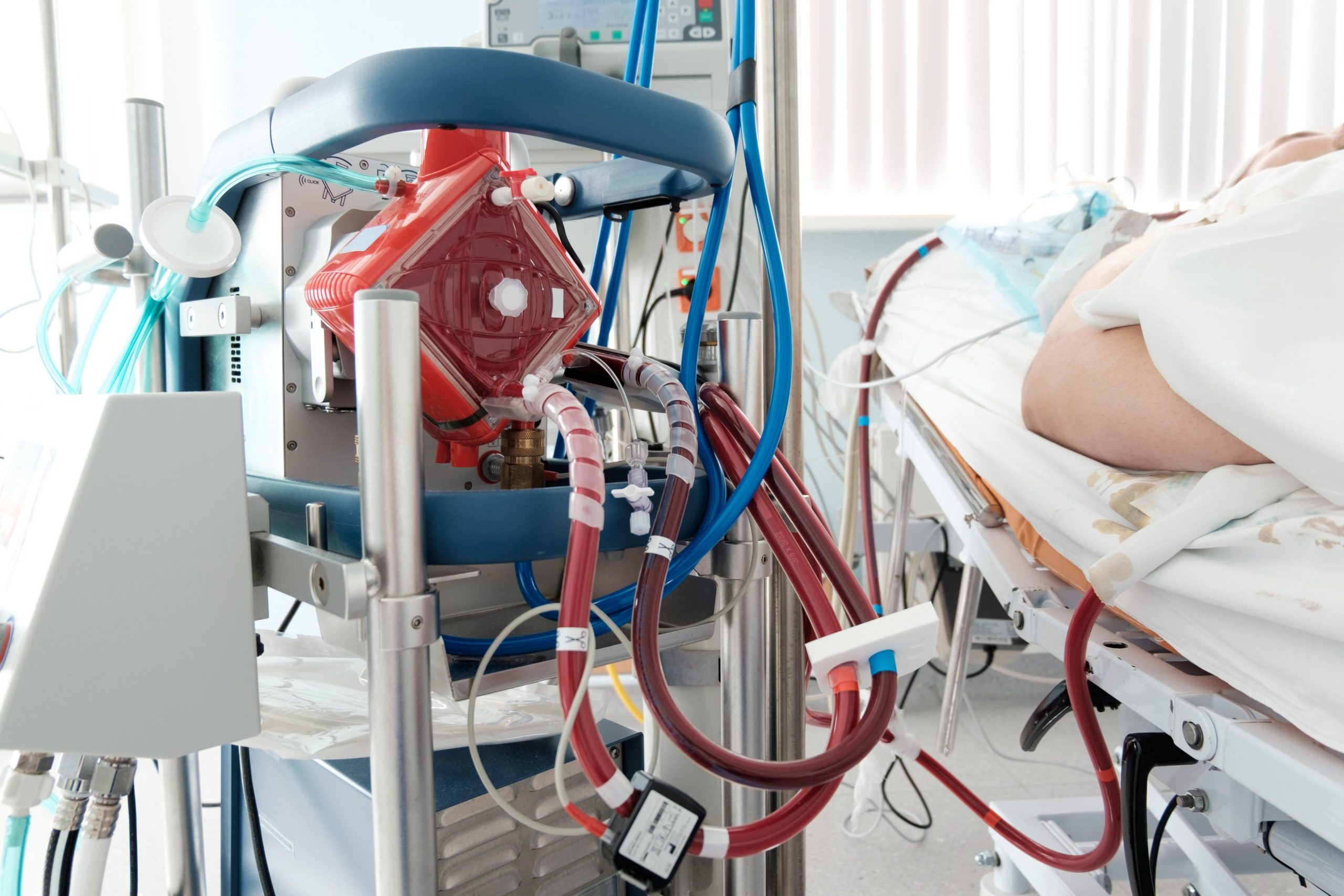
ECMO is a machine that helps patients with life-threatening illness or injury breathe by allowing the heart or lungs to rest while simulating their functions. It involves pumping blood out of the body, sending it through devices that feed it oxygen and then returning it to the body.
“The goal is to really get people thinking about where some disparities within critical care might live,” said study author Dr. Anuj Mehta, an assistant professor of medicine within the Division of Pulmonary Sciences and Critical Care Medicine at Denver Health and Hospital Authority and the University of Colorado School of Medicine.
“The next step is to think about how we can investigate those disparities with better data and better sources, which supports the long-term goal of ensuring equitable care,” Mehta said in an NIH news release.
The researchers used health insurance data from more than 2 million U.S. adults who had severe respiratory illness between 2016 and 2019. All of the patients had first received mechanical ventilation, having a breathing tube inserted into the airways to help their bodies get enough oxygen.
Among those who received mechanical ventilation, more than 18,700 also received ECMO.
Researchers found that men received ECMO more often than women, even if they had the same type of insurance and income level. Men were 64% of those receiving ECMO, compared to 36% who were women. Men also were 55% of those who just received mechanical ventilation, compared to 45% who were women.
About 38% of those who received ECMO had private insurance, while 37% had Medicare. About 18% had Medicaid and 7% had other insurance or possibly no insurance.
Among patients who only received mechanical ventilation, 58% used Medicare, 17% used Medicaid, 17% used private insurance and 8% had other insurance or no insurance.
About 25% of those who received ECMO were from higher income areas and 25% from lower-income areas. Still, just 17% of patients who only received mechanical ventilation came from high-income areas, compared to 33% of patients from lower-income areas, the authors noted.
The findings are associations and do not necessarily mean that doctors intentionally refer some patients over others for advanced care, Mehta cautioned.
Multiple factors could explain these variations, the authors said.
Patient preferences and implicit bias are among those factors. It also could be that living near or being more likely to be referred to an advanced medical center that provides ECMO is a third reason.
Yet, even after controlling for access to ECMO, such as looking at patients who received care at the same hospital, the researchers still found disparities.
“These findings add to existing research that shows more work is needed to both understand and alleviate disparities in advanced pulmonary care,” said James Kiley, director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute (NHLBI).
ECMO was created about 50 years ago. It has mixed outcomes in prolonging life compared to other types of respiratory care. One type of ECMO takes over for the lungs, while another type simulates the heart and lungs. The latter is often used for those recovering from heart surgery, while the other may provide temporary breathing assistance to patients waiting for a lung transplant or those recovering from severe respiratory failure.
The findings were published in the Annals of the American Thoracic Society.
More information
The U.S. National Library of Medicine has more on ECMO.
SOURCE: U.S. National Heart, Lung, and Blood Institute, news release, April 6, 2023
Source: HealthDay

Leave a Reply